Relief From Osteoarthritis Pain
Professor Jari is one of the pioneers of Mako Robotic arm assisted surgery having very successfully performed the first MAKO Total Knee Replacement and the second MAKO partial knee replacement in the North-West of England. The two patients concerned have kindly provided their video testimonials below.
Over the years, knee replacement techniques and instrumentation have undergone countless improvements. Mako Robotic-Arm Assisted Surgery System is an example of how technology is transforming the way joint replacement surgeries are being performed.
When you hear ‘robotic-arm assisted technology,’ it’s important to understand that the Mako Robotic-Arm doesn’t actually perform the surgery. Surgery is performed by Professor Jari, who uses the Mako System software to pre-plan the surgery. Professor Jari then guides the Mako robotic-arm to remove diseased bone and cartilage during the operation. Finally, Professor Jari will insert the knee replacement.
Mako Technology was designed to help surgeons in their efforts of providing personalized surgical experience, with each surgical plan being based on a patient’s specific diagnosis and anatomy.
All inclusive package
Professor Jari has created a Unique and Exclusive Package of benefits for all of his Private self-pay patients who undergo MAKO Robotic Assisted Total or Partial Knee replacement Surgery which are ALL included in the cost of the special Fixed Price Package.
Advantages over other systems
The advantages of less invasive surgery are:
- To allow quicker rehabilitation of the knee due to the decreased soft tissue and bony trauma.
- There is also less bleeding which can lead to less swelling and less pain, which contributes to the quicker rehabilitation.
- A greater range of motion can be achieved compared to a conventional approach. There is a potentially quicker return to function.
Taking all the above into account, a potential quicker return to function can be achieved, resulting in a shorter length of stay in the hospital of between 1 to 3 days.
By reducing the length of stay in a hospital, this has a secondary effect including to reduce the risk of hospital-acquired infections including MRSA as well as potentially reducing the risks of DVT and pulmonary embolus due to early mobilisation.
My patients who undergo knee replacement surgery follow an accelerated rehabilitation programme which commences on the day of surgery. This includes use of a CPM (Continuous Passive Motion) machine, immediate range of motion exercises, quadriceps strengthening, hyper-extension stretching and early walking (preferably on the day of surgery). This is combined with a specific and effective pain-relieving drug regime devised by Professor Jari which he has been successfully using with his patient for many years.
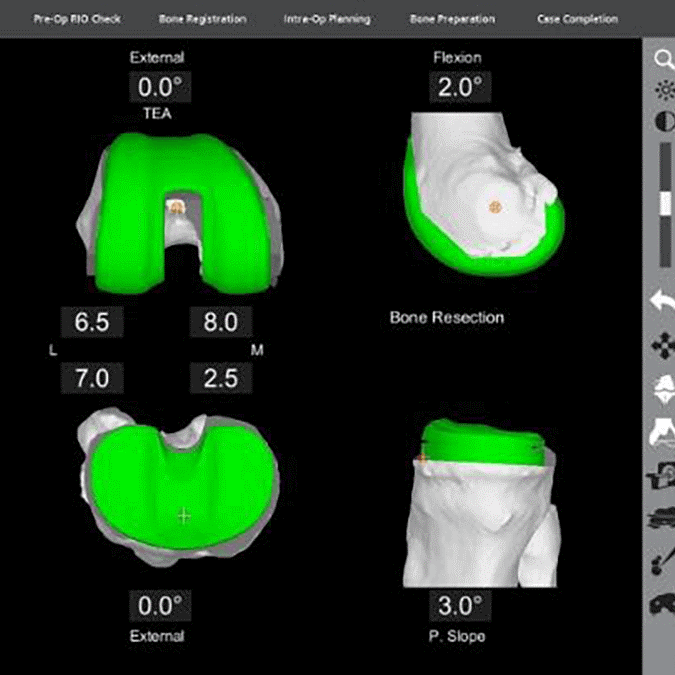
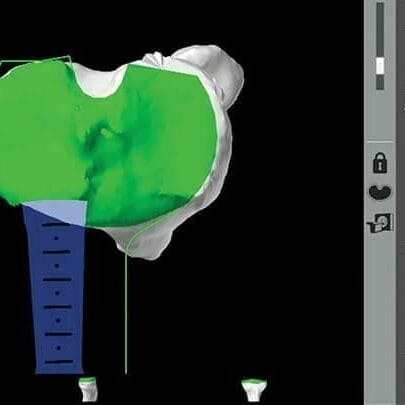
Personalised Plan
It all begins with a CT scan of the patient’s knee joint that is used to generate a 3D virtual model of patient’s unique anatomy. This virtual model is loaded into the Mako system software and is used to create the patient’s personalised preoperative plan.
In the Operating Theatre
In the operating theatre, Professor Jari uses Mako system to assist in performing the surgery based on the patient’s personalized preoperative plan. The Mako system also allows the Professor Jari to make adjustments to the patient’s plan during surgery as needed. When the Professor Jari prepares the bone for the implant, the Mako system guides him within the pre-defined safe areas and helps prevent the him from moving outside the safe planned boundaries. Overall this helps safely provide more accurate placement and alignment of the implant as per the patient’s personalised plan and intra-operative adjustments undertaken by Professor Jari.

After Surgery
After surgery, Professor Jari, nurses and physiotherapists set goals with the patient to get the patient back on the move. They closely monitor the patient’s condition and progress. Professor Jari will also obtain and review post-operative x-rays of the new knee.
Patient Experience
Firstly, I cannot begin to explain what a difference having both knees replaced has done to me personally and am writing this testimonial to highly recommend Prof Sanjiv Jari whom specialises in Orthopaedics at Spire Manchester Hospital.
I have recently had 2 Mako Robotic Assisted Total Knee Replacements with Prof Jari, my left was done on 26th August 2022 (I’m nearly 6 months post-op) and more recently my right was done on 6th January 2023 (6 weeks post-op) and it is time for an amazing update on my progress!
Before having my first knee replacement I felt very apprehensive and worried about the whole procedure, this soon changed once meeting Prof Jari. He gave me his time and listened to how everything was affecting me and having an impact on my day-to-day living. After deciding that this was the correct procedure to have and that it was deemed appropriate, he reassured me massively and explained the whole procedure at great lengths and in great detail, making sure I fully understood everything (do’s, don’ts, benefits etc).
On the day I was admitted for my first knee replacement surgery, I was so nervous, but Prof Jari came to see me before going for surgery and again we spoke about what was going to happen during the procedure and answered any questions that I had, which again, made me feel so much more at ease. During my 2-night stay at the Spire Manchester Hospital, Prof Jari came to see me during both days. Prof Jari also recommends his patients use a CPM Machine (continuous passive motion) after surgery, and I can safely say the advantages I felt using this post-op is that it helped improve my range of motion and helped decrease pain and prevented me from stiffening up.
I was so surprised at the result of my surgery and how it made me feel, I couldn’t believe how quickly I was back on my feet and able to do my daily routines again. I even went back to work 4 weeks after having surgery. During this time and after speaking with Prof Jari previously, I knew that my other knee also needed to be replaced and again, due to my successful progression after my first knee replacement, Prof Jari advised me to get booked in for my 2nd surgery.
I was admitted for this on 6th January 2023 (4 months after 1st knee replacement), Prof Jari never ceased to amaze me. Although I had recently had my first operation, he again dedicated his time in coming to see me before surgery, explaining the procedure and again answering any questions that I had. This was another success, I was up and about even quicker after this surgery, doing my day-to-day tasks/routine and on this occasion, returned back to work after 3 weeks. On both occasions I was able to drive myself after 4 weeks of having each one done (this will of course be different for everyone).
Before having surgery and from the time I got out of bed, I was in constant pain that had to be managed with prescribed medication. My daily tasks and routines became less and less due to the restrictions I was experiencing. My hobbies and interests had become non-existent due to having so much trouble in walking and standing for long periods at a time and this is why I’m so excited and delighted to share my experience with everyone as I can’t believe how far I have come in 6 months.
I want to say a HUGE thanks to Prof Jari and all his team in theatres and also not forgetting his secretary Stephanie Snowball, the relationship I have experienced with both throughout my whole experience has been amazing, warm, friendly and very professional.
Prof Jari’s manner post-op and aftercare is second to none, it is very apparent that he is a very caring person towards his patients and passionate in what he does and the results he achieves are unbelievable and amazing and that is why I am wanting to share my successful story with everyone.
“Prof Jari you have helped me get my quality of life back again, which at one point I couldn’t see beyond the pain, limping, and hobbling around, and this was really getting me down, but now I am where I thought I would never be again. It is a pleasure to get up in the morning, being completely pain free and I’m so very grateful and thankful to you for making this big difference in my life, this really does mean so much to me as I am only 52 and want to also say thank you for all your support that you have given me”.
Sharron Ford, Manchester
February 2023
Regarding my recent surgery for a part knee replacement done by Professor Jari using the Mako-robot, the overall experience has been first class from the diagnostic to the treatment pre-op and more importantly post-op. The arrangement of bookings for x-rays, scans to consultations has been excellent.
The staff have gone beyond their duty to make me feel totally at ease with everything from choosing which Hospital to making appointments and choosing my physio. Especially Claire the practice manager who went above and beyond in helping me with regards my Insurance questions and any worries/concerns that I may have had.
It has now been 8 weeks since my operation and I wish I would have had it done sooner because there is no longer anymore pain in my left knee, I feel like a completely different person now and look forward to getting back to my regular hobbies that I couldn’t do because of the pain I was in. Here’s to happy golfing/swimming/cycling.
I would certainly recommend Professor Jari (TheKneeDoc) for whatever treatment that you may require.
Many thanks for everything
Professor Jari was fortunate enough do the first MAKO knee replacement in the North West and now he is one of the surgeons who have collectively passed 2000 successful MAKO hip and knee replacement cases at Spire Manchester Hospital in 2024

Make An Enquiry
Or contact us directly
[email protected]
0161 445 4988
