What is Osteoarthritis?
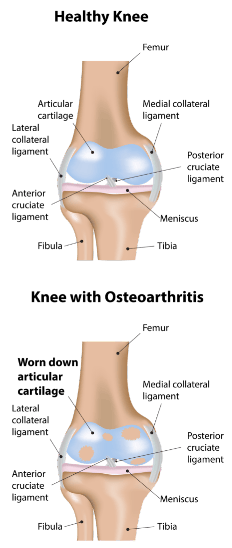
Arthritis is a condition affecting joints of the body and involves the destruction or loss of the lining (articular) cartilage of the joint. It is usually a degenerative condition associated with ‘wear and tear’ and a normal part of aging.
The most common type of arthritis is degenerative osteoarthritis, the incidence of which increases with age. There are, however, other types of arthritis that are generically termed inflammatory arthritis and include conditions such as rheumatoid arthritis and other connective tissue-related arthropathies. The knee is the largest synovial joint in the body and is commonly affected by arthritis as is the hip and the ankle, as well as the foot. Arthritis is more common in weight-bearing joints and so is more frequently seen in the lower limb than the upper limb. Arthritis can run in families but is not specifically genetically predisposed. Arthritis of the knee is more common in people who expose their joints to repetitive micro-trauma, of which weight-bearing is a simple example. This will slowly overload the joint, especially if the person is overweight. It is thought that people involved in many years of sports, which include running, twisting and jumping can also be predisposing themselves to an increased risk of arthritis in future years. There is no doubt that various types of acute trauma to the knee, such as fractures, dislocations, and major ligament injuries, as well as direct damage to the lining (articular) surface of the knee joint, can lead to accelerated arthritis development in the years to come.
Biomechanics
Normal alignment of the lower limb results in weight-bearing forces of the body going through the medial (inner) compartment of the knee. Therefore medial compartment arthritis is the usual starting point for knee arthritis as this is the compartment that is being continually loaded.
Any condition that changes the loading pattern and alters the mechanical axis of the leg can result in arthritis distribution in other compartments of the knee. This can occur in fractures that heal with malalignment or even with the removal of meniscus tissue which will result in increased force being put through the articular cartilage in the affected compartment.
The increase force applied to the articular cartilage over time causes breakdown of the articular cartilage and the development of arthritis.

Clinical Assessment
The clinical assessment of a patient with knee arthritis involves taking a detailed history which will include
- Location of pain.
- The severity of pain.
- When the pain comes on – activity-related, rest pain, or night pain.
- Swelling of the knee.
- Walking distance.
- Activity restriction due to symptoms.
- The type of analgesia/anti-inflammatories used and their effect on the symptoms.
- The effect of any previous treatment that has been given – for example, physiotherapy or injections.
- Any history either in the individual or the individual’s family of inflammatory arthritis or gout.
The next step is to examine the knee joint as well as assess the hip joint and the lumbosacral spine both of which can cause radiating pain to the knee. During the examination, the patient’s gait (walking pattern) is assessed and any deformities of the knee in all the planes are documented.
Investigations
Investigations for arthritis usually entail weight-bearing radiographs of the knee and also a long leg standing alignment x-ray of the leg to show the axes of the leg and knee.

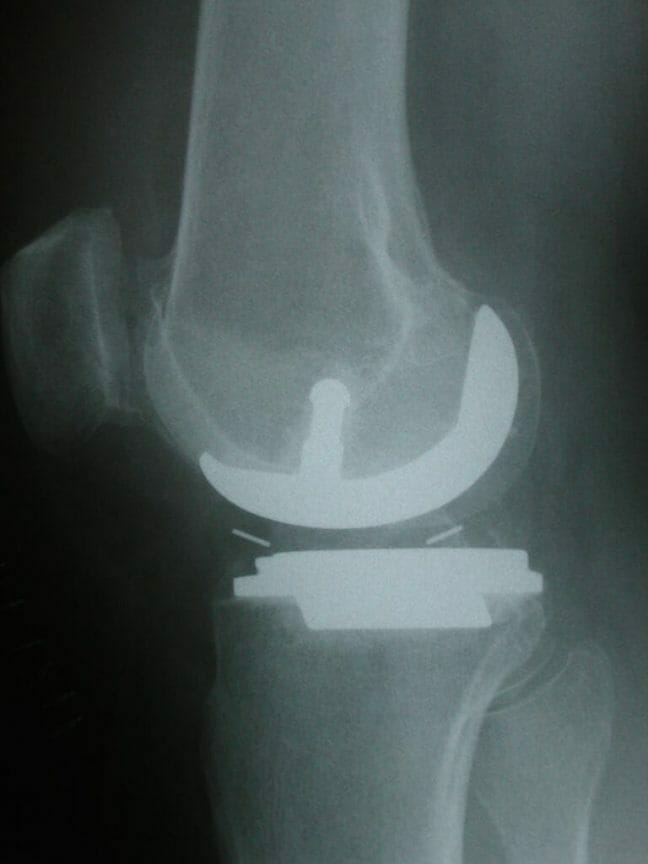
AP x-ray of the knee showing gross lateral compartment osteoarthritis with total loss of lateral joint space.

AP x-ray of the knee shows early medial compartment osteoarthritis with mild medial joint space narrowing.

Skyline view of patellofemoral joint showing patellofemoral arthritis with loss of lateral patella joint space and lateral tilt of the patella.
Treatment
Make An Enquiry
Or contact us directly
[email protected]
0161 445 4988